Recent Publications
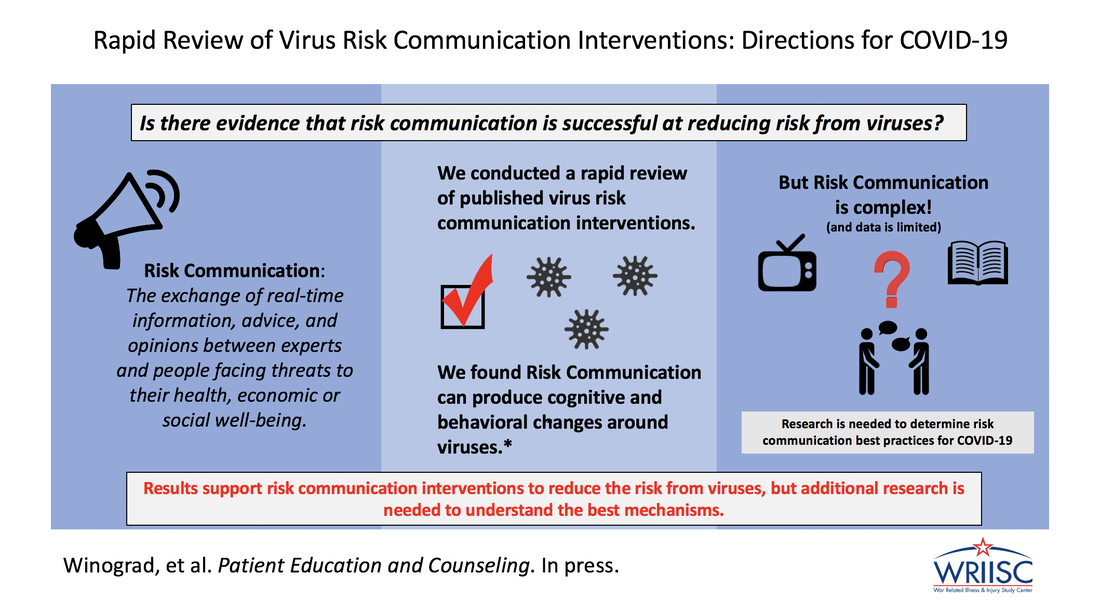
The world is facing the unpresendented pandemic of coronavirus disease 2019 (COVID-19). While risk-communication is an important mechanism for controlling pandemic events, little is known about effective methods of virus risk communication. We therefore conducted a rapid review of risk communication interventions to mitigate risk from viruses to determine the efficacy of such interventions. Thirty-one articles were included in the final review. This study showed risk communication can be efficacious in producing cognitive and behavior changes around viruses. There was no consistent best intervention approach. Tailoring risk communication toward a target population, in comparison to not tailoring, was related to better outcomes.
Ultimately, results support risk communication interventions as efficacious options in reducing risk from viruses.
Ultimately, results support risk communication interventions as efficacious options in reducing risk from viruses.
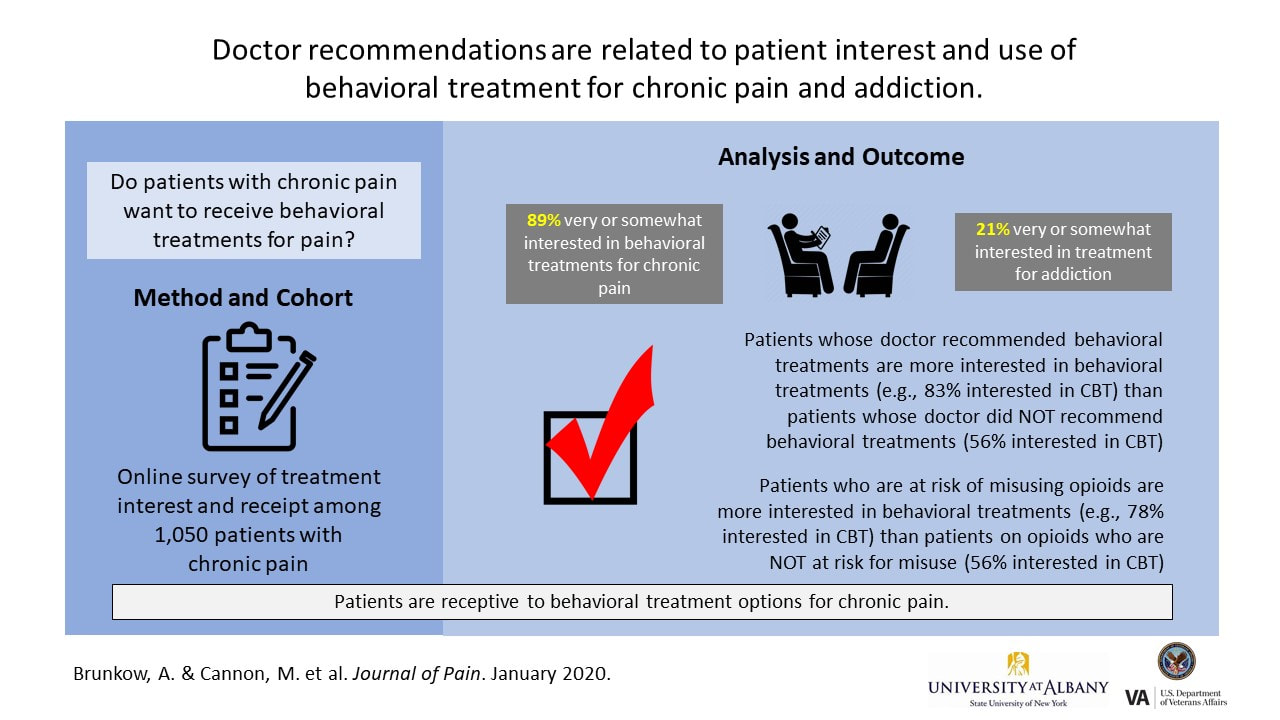
Chronic pain is a disabling health condition that affects many Americans. Chronic pain is sometimes treated with opioid pain medication, but problems with this treatment include lack of evidence of long-term benefit and risk of addiction and overdose. Given the epidemic of opioid overdoses, behavioral, non-medication therapies (like cognitive-behavioral therapy, health coaching, and other treatments) are the treatments of choice for chronic pain, but we do not know whether patients want to receive these. This study was an anonymous online survey of over 1000 people with chronic pain. Participants were asked whether they had used, were interested in, or been recommended a range of behavioral treatments or medication for chronic pain and addiction. This study found that patients are interested in non-medication treatment options for chronic pain, including those who may be at risk for misusing opioids. Patients who received treatment recommendations from their doctors were more likely to be interested in receiving those treatments than patients who did not receive treatment recommendations. Study findings highlight the association between doctor recommendation and patient interest and receipt of a treatment. Doctors are encouraged to discuss the many non-medication treatment options for chronic pain management with their patients rather than assume patients prefer to treat chronic pain solely with medication.

Integration of Common Sense Model and Self Efficacy In this study we reviewed research articles to understand how two health psychology theories – the Common Sense Model and self-efficacy – were related to health outcomes (like quality of life) and health behaviors (like taking medication). We did this review because the theories are used a lot in health psychology research, but no one had studied whether both theories were useful when included in the same statistical models.
The Common Sense Model is a theory that describes how people understand health conditions. It suggests they use information like the name of the condition, its symptoms, its cause, its consequences, how long they might have the condition, and whether or not the condition can be controlled. Self-efficacy is a theory that suggests people are more likely to do a behavior, like exercise, if they are confident that they can be successful. The idea of self-efficacy is not specific to health, but it is used in a lot of health research.
After reading over 100 papers, we included 25 studies in the review. Those studies included 55 statistical models. We found that both the Common Sense Model and self-efficacy were related to health outcomes and health behaviors. The Common Sense Model was related to health outcomes more often (in 73% of models). Self-efficacy was related to health behaviors more often (in 76% of models). We concluded that researchers should continue to use both the Common Sense Model and self-efficacy in health psychology research because both provide useful information.
The Common Sense Model is a theory that describes how people understand health conditions. It suggests they use information like the name of the condition, its symptoms, its cause, its consequences, how long they might have the condition, and whether or not the condition can be controlled. Self-efficacy is a theory that suggests people are more likely to do a behavior, like exercise, if they are confident that they can be successful. The idea of self-efficacy is not specific to health, but it is used in a lot of health research.
After reading over 100 papers, we included 25 studies in the review. Those studies included 55 statistical models. We found that both the Common Sense Model and self-efficacy were related to health outcomes and health behaviors. The Common Sense Model was related to health outcomes more often (in 73% of models). Self-efficacy was related to health behaviors more often (in 76% of models). We concluded that researchers should continue to use both the Common Sense Model and self-efficacy in health psychology research because both provide useful information.
|
|

Role of Beliefs & Behaviors in Medically Unexplained Symptoms Medically Unexplained Symptoms (MUS) can be highly disabling. Research on coping with MUS has shown that beliefs about MUS and how individuals respond to their symptoms may contribute to disability. However little is known about which specific thoughts and behaviors are related to better functioning. As part of a large study, Dr. Lisa McAndrew and her team asked Veterans with MUS about how they think about their symptoms, how they respond to their MUS, and their level of functioning. The researchers found that Veterans who saw their MUS as controllable and understandable were functioning better compared to those who saw their MUS as threatening (e.g., having severe consequences). The researchers also found that these beliefs were related to certain behaviors. For example, those who saw their MUS as threatening were more likely to limit the activities they engage in, which was related to more disability. On the reverse side, seeing MUS as controllable and understandable was related to less limiting behavior and less push-crash behavior (i.e., a cycle of avoiding activity followed by extreme bouts of activity that leave an individual burned out). Less limiting and less push-crash behavior was related to better functioning. The findings of this study suggest some specific ways that might be helpful for Veterans to cope with the symptoms of MUS, and improve functioning.
| Sullivan, N., Phillips, L.A., Pigeon, W.R., Quigley, K.S., Graff, F., Litke, D.R., Helmer, D.A., Rath, J.F., & McAndrew, L.M. (2019). Coping with medically unexplained physical symptoms: The role of illness beliefs and behaviors. International Journal of Behavioral Medicine. doi: 10.1007/s12529-019-09817-z | |
| File Size: | 763 kb |
| File Type: | |

Longitudinal relationship between onset of physical symptoms and disability To understand the relationship between pain and disability as they develop, Dr. McAndrew and her team followed 790 military personnel returning from deployments in Iraq and Afghanistan. Military personnel were assessed before, immediately after, 3-months after and 1-year after their deployment. The researchers found that for those who experienced an increase in pain symptoms during deployment also reported increases in their disability at later time points. Interestingly, the reverse was not found; disability reported during deployment did not lead to later increases in pain. In other words, disability did not cause acute pain to become chronic, as has been commonly assumed. The results of this study suggest the need for new models of how acute pain becomes chronic.
| McAndrew, L.M., Helmer, D.A., Lu, S-E., Chandler, H.K., Slotkin, S., Quigley, K.S. (2018). Longitudinal relationship between onset of physical symptoms and functional impairment. Journal of Behavioral Medicine. dx.doi.org/10.1007/s10865-018-9937-4 | |
| File Size: | 635 kb |
| File Type: | |
Communication about Medically Unexplained Symptoms Dr. McAndrew and her team reviewed the literature on patient-provider relationships in the context of medically unexplained symptoms. Their review suggests that the key to improving patient-provider relationships is for the patient and provider to negotiate a shared understanding of the patient’s symptoms. Having such a shared understanding of illness perceptions, consequentially, becomes the foundation for developing an effective treatment plan.
| McAndrew, L.M., Friedlander, M., Phillips, L.A., Santos, S., & Helmer, D.A. (2018). Concordance of Illness Perceptions: The key to improving the care of medically unexplained symptoms. Journal of Psychosomatic Research. dx.doi.org/10.1016/j.jpsychores.2018.05.015 | |
| File Size: | 385 kb |
| File Type: | |

Evaluating Challenges for Improving Medically Unexplained Symptoms via Communication Effective patient-provider-communication is a key aspect of care. Veterans experiencing Medically unexplained Symptoms (MUS) reported on their communications with primary care providers about their illness. While both interpersonal skills and MUS discussion (i.e., illness and treatment factors) were significantly related to care satisfaction, only MUS discussion was related to treatment adherence. Results communicate the importance of patient-provider interactions in Veteran MUS treatment.
| Phillips, L. A., McAndrew, L., Laman-Maharg, B., & Bloeser, K. (2017). Evaluating challenges for improving medically unexplained symptoms in US military veterans via provider communication. Patient Education and Counseling. | |
| File Size: | 589 kb |
| File Type: | |
Upcoming projects: Protocols
Comparative Effectiveness of Behavioral Interventions for MUS: A Meta-Analysis |
| ||||||